Volume 2, Issue 12
December 2022
Transoral Excision of Sublingual and Submental Dermoid Cyst of the Floor of the Mouth: A Case Report
Abdulaziz Alwatied, Feras Moslem
DOI: http://dx.doi.org/10.52533/JOHS.2022.21217
Keywords: dermoid cyst, intraoral, surgery, sublingual
Background: A dermoid cyst is a cystic lesion of developmental origin and uncertain etiology that rarely affects the floor of the mouth. It usually presents as a non-tender, slow-growing swelling in the sublingual region.
Case presentation: A large lesion was found in the sublingual and submandibular regions of a 15-year-old female patient who presented to our clinic with the chief complaint of a sublingual mass that had been present for many years but had enlarged over the last year. Computed tomography (CT) scans revealed a giant cystic mass that was a 4.6 x 3.3 cm flask-shaped cystic lesion with a non-enhancing wall in the midline of the sublingual space. Magnetic resonance imaging (MRI) with contrast revealed a well-defined cystic mass with heterogeneous fluid on all sequences. The histopathology report was suggestive of a dermoid cyst. The intraoral approach was preferred for surgery, and no recurrence or complaints were detected during the follow-up period.
Conclusion: The pathological diagnosis of the presented case was an epidermoid cyst. For giant dermoid cysts, a surgical incision is considered an effective treatment of choice. This offers a good prognosis and very low chances of recurrence. To achieve the best cosmetic effects, an intraoral technique should be chosen whenever possible.
Introduction
Dermoid cysts, a benign cutaneous developmental aberration, are uncommon in the head and neck, with an incidence ranging from 1.6% to 6.9%, and they account for less than 0.01% of all oral cavity cysts. They are caused by the trapping of ectodermal components along the lines of embryonic closure (1-3). The majority of dermoid cysts of the oral cavity's floor are located in the midline, such as sublingual (52%), and submental (26%), with 16% involving multiple spaces in the floor of the mouth region (submental, sublingual, and submandibular), and only 6% involving lateral neck cysts (4). Dermoid cysts are typically asymptomatic unless they dramatically enlarge, causing pain or trouble breathing, speaking, eating, or seeing, depending on their location. The pathophysiology of a midline cyst of the floor of the mouth, however, is not fully understood, but dysontogenetic (entrapment of mesoderm during midline fusion), traumatic, and thyroglossal anomaly causes have been suggested. Most lesions become clinically evident from 15 to 35 years of age. The treatment of choice is the removal of the entire cyst via surgical excision. Here we report a case of a giant sublingual dermoid cyst on the floor of the mouth of a 15-year-old female child that was successfully removed by surgical midline incision.
Case report
A 15-year-old female presented with persistent swelling beneath the tongue and a visible mass under the chin of a 4-year duration. The patient first noticed the mass underneath her tongue when she was 12 years old. The swelling increased slowly until the patient was 14 years old, after which the patient reported a dramatic increase in the swelling’s size, which became apparent under the chin.
The patient did not report any associated dysphagia, dysphonia, or dyspnea and did not report any episodes of fever or other systemic illness, and she was not on any regular medication.
On examination, there was a 5x4 cm midline swelling apparently in the submental area. On inspection, the lesion did not exhibit any extraoral skin color changes or any extraoral sinus discharge. On palpation, the lesion was soft and non-pulsatile, and its surface was smooth with diffuse edges. The mass was not attached to either the underlying or overlying structures and could be brought into the oral cavity. The surrounding skin was normal, and examination showed no lymphadenopathy (Figure 1).

Figure 1: Pre-operative photo of the swelling in the submental area
Oral examination revealed a sublingual swelling covered by normal mucosa and a slightly elevated tongue. The bilateral submandibular ducts (Wharton’s duct) appeared normal. All laboratory investigations were within normal limits. A maxillofacial computed tomography (CT) scan with contrast revealed a 4.6 x 3.3 cm cystic flask-shaped lesion with a non-enhancing wall in the midline of the sublingual space. No loculations or septations were seen on the CT scan (Figure 2A). Magnetic resonance imaging with contrast revealed a well-defined cystic mass with heterogeneous fluid on all sequences (Figure 2B). The mass was hyper-intense on T2-weighted images. The mass was located superior to the mylohyoid muscles, had no soft-tissue components, and did not display local infiltration. There was a moderate mass effect where the lesion slightly compressed the airway (Figure 2).

Figure 2: A) Maxillofacial CT reveals cyst in the lingual space. B) Transverse section on T2 Weighted MRI revealing a hyper-intense cystic mass in the sublingual space
All the investigations were suggestive of a sublingual dermoid cyst. Under general anesthesia and with nasotracheal intubation, the patient underwent surgical removal of the mass. A midline incision from the base of the tongue to the area between the openings of the two submandibular gland ducts was made after infiltrating the area with 2% lignocaine hydrochloride and 1:80,000 epinephrine for hemostasis. Dissection was performed until the cyst wall could be seen (Figure 3). Special care was paid to avoid any injury to the bilatera submandibular gland ducts. This was followed by a dissection of the cyst from the surrounding tissues. The cyst was then delivered into the oral cavity and enucleated with no evidence of rupturing the cystic wall (Figure 4). The cyst was removed with an intact capsule (Figure 5).

Figure 3: Intra-operative image of the dissection showing the cyst wall

Figure 4: The excised lesion (capsule like) was delivered through the oral cavity

Figure 5: The lesion measuring 4x5 cm
The wound was then closed in layers and sealed with interrupted sutures. The postoperative period and healing were uneventful. A one-year follow-up showed no recurrence. The mass was histopathologically identified as a 5 x 4.5 cm cystic mass containing yellow granular material. The cyst wall was lined with keratinized stratified squamous epithelium and contained mature sebaceous glands and hair follicles, thus confirming the diagnosis of a true dermoid cyst (Figure 6).
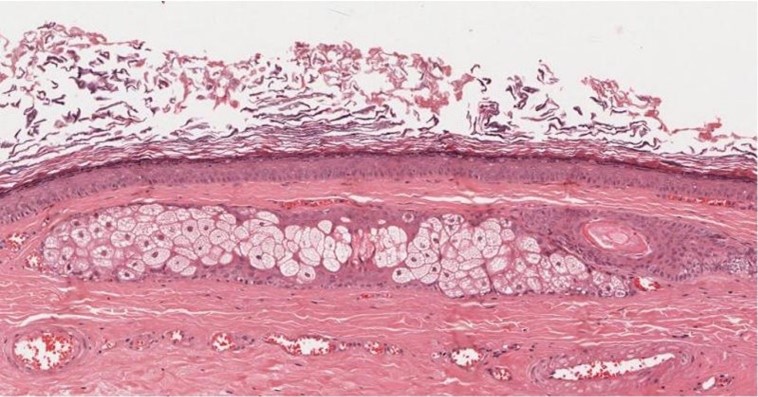
Figure 6: Histopathological slide showing the cyst wall lined by ortho-keratinized stratified squamous epithelium with a prominent granular cell layer. There are sebaceous glands and small hair follicles in the connective tissue (H&E stain, 40X).
Discussion
Cystic malformations lined with squamous epithelium are classified into three groups based on whether they are lined with simple squamous epithelium (epidermoid), skin adnexa are found in the cystic wall (dermoid), or other tissues, such as a muscle, cartilage, or bone, are present (teratoid) (5). Both dermoid and epidermoid cysts are cystic choristomas filled with keratin, cholesterol clefts, or degenerated blood components and produced by keratinizing squamous epithelium; but whereas true dermoid cysts have skin appendages, sebaceous or sweat glands, or purulent hair on their walls, an epidermoid cyst's wall does not have these appendages (6). Ectoderm, mesoderm, and endoderm-derived tissue structures may be present in the teratoid cyst's lining and wall. All three types of cysts have a cheesy white-grey or yellowish content formed by shed keratin and sebaceous material in their lumen (7). In our cases, the presence of keratinized stratified squamous epithelium and mature sebaceous glands and hair follicles points to the diagnosis of dermoid cysts.
Anatomically, the cysts can be divided into three regions: sublingual (above mylohyoid and genioglossal muscles), submental (between geniohyoid and mylohyoid muscles), and submandibular (lateral to the musculature) (8, 9). In the present case, the cyst was located above the mylohyoid muscle and designated as a sublingual type. The lateral brows are where dermoid cysts on the head and neck are most frequently detected. The floor of the mouth is the second zone, and it accounts for 6.5% of all the dermoid cysts in the head and neck region, making these uncommon entities (10). Like our patients, dermoid cysts typically occur in the midline and anterior portions of the oral cavity and tend to manifest in the second or third decade of life (11, 12); however, they can present at any age with an equal frequency of occurrence for both genders (13). In most cases, the cyst is large because the period of time until a hospital visit is delayed, and the cyst at that time is often huge.
Clinical signs and symptoms mainly depend on the affected anatomical sites and vary considerably. Although most cases are asymptomatic, such as ours, clinically, the dermatoid cyst in the floor of the mouth is a painless, slow-growing lesion; however, pain can occur if a secondary infection is present. A dermoid cyst has a doughy texture and is frequently soft and well encapsulated, with no associated lymphadenopathy. Meyer et al. (5) proposed that, regardless of the microscopic characteristics, the appearance of a doughy cyst on the floor of the mouth on clinical examination was adequate for a dermoid cyst diagnosis. In our case, the patient first noticed the mass underneath her tongue when she was 12 years old. The mass was slowly growing until the patient was 14 years old, after which the patient reported a dramatic increase in the swelling’s size, which became apparent under the chin. The sudden increase in size is postulated to be due to the onset of puberty when there is an increase in the secretion of sebum from the sebaceous glands. Acute enlargement can also occur due to infection, which leads to the blockage of the salivary glands involved in the cyst, or by the implantation of oral microbes into the cyst through trauma (14).
Typically, dermoid cysts are asymptomatic but can cause complications such as inflammation, dysphagia, dystonia, disorders of swallowing, chewing, or vocal function, and airway encroachment due to mass effects (15, 16). Those complications are mostly related to cyst size. Submental cysts bulge into the submental area, giving the impression of a “double chin” (17), as present in our case. However, our patient was asymptomatic in this instance since there was neither a secondary infection nor displacement of the tongue.
It is critical to differentiate dermoids on the floor of the mouth from ranulas due to the difference in management; only the latter can be successfully managed with marsupialization and/or excision of the affected salivary gland (18). Other differential diagnoses include infections, lymphadenopathies, and duplications of foregut cysts. To achieve a correct diagnosis, specialized imaging examinations such as CT, MRI, and histopathological examinations should be carried out (19). Diagnostic imaging plays a pivotal role in the anatomic localization of the mass on the floor of the mouth and, therefore, helps in guiding surgical planning. As in our case, a T2-weighted MRI is recommended to depict the relationship between a cystic lesion on one side and the geniohyoid and mylohyoid muscles on the other (20, 21).
The effective treatment of choice for dermoid cysts is surgical enucleation. Depending on their location in relation to the mylohyoid muscle, the lesions can be exposed via an intraoral or extraoral approach (8). An intraoral approach is preferred in cases of cysts above the mylohyoid muscle, as in our case, whereas an extraoral technique is preferred in cases of large dermoid cysts affecting the submandibular and submental spaces and in the presence of an infection that could compromise the patient’s airway. We managed to remove this relatively large mass purely via an intraoral approach, and hence we were able to avoid cosmetic problems. A combined intraoral and extraoral approach was advised to expose and excise massive lateral dermoid cysts in the Gulati et al. (22) report. Some authors prefer decompression of the cyst before excision. Some authors prefer decompression of the cyst before excision. Extravasation of the cyst content during excision can cause postoperative inflammation. A thorough irrigation of the area should be undertaken in such situations in order to avoid postoperative inflammation. Recurrences are unusual after total surgical excision. Spontaneous rupture and malignant transformation of a dermoid cyst are rare and usually occur in the ovaries and testes; less than 2% of cases of malignant transformation have been reported in previous studies (23). In our case, no recurrences were observed in the next year. Based on our case, it can be stated that the dermoid on the floor of the mouth is easily removed intraorally. It gives a better cosmetic and functional result with a short recovery time.
Conclusion
The pathological diagnosis of the presented case was an epidermoid cyst. For giant dermoid cysts, a surgical incision is considered an effective treatment of choice. This offers a good prognosis and very low chances of recurrence. The definitive treatment for sublingual dermoid cysts is surgical excision via an intraoral approach. To achieve the best cosmetic effects, an intraoral technique should be chosen whenever possible
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
The patient written consent was obtained to publish this report anonymously. The ethical committee of King Saud Medical City approved the publication of this case report.
Data availability
Data that support the findings of this case are embedded within the manuscript.
Author contribution
The authors contributed to drafting, writing and proofreading the case report.
